How Long Can an Elderly Person Live Without Eating
Summary of This Article
Find a Support Group
Few things are harder than watching a loved one skid away considering of a life-limiting illness. The feel is even more than challenging when family members and caregivers notice that their hospice patient stops eating and drinking at the end of life.
A dying patient's needs for food and water are far different from those of a salubrious, active person.
Families may worry:
- Are we giving upward on our loved one if we don't try to feed them or offering water/fluids?
- What is our loved one's hazard of survival without water or food in hospice intendance? How long tin a hospice patient alive without food and water?
- Our family unit traditions revolve around food and drink as symbols of loving care. Are nosotros taking away the dearest if nosotros take away nutrition and hydration? Are we letting our loved one starve to death?
- Will withholding food and water at the end of life crusade pain for our loved i?
- What can we do to make certain our loved one does not endure?
Exist Guided by the Trunk's Gradual Decline
A dying patient's needs for food and water are far different from those of a salubrious, active person. Equally the cease of life nears, the body gradually loses its ability to digest and process foods and liquids. As organs and bodily functions shut downward, minimal amounts of nutrition or hydration/liquids might exist needed, if at all.
Standing to offer food and water, or opting for artificial nutrition or hydration (ANH)—such every bit nasal (NG) or stomach (PEG) feeding tubes or Four fluids for hydration—can actually complicate the dying process and lead to other health bug.
VITAS Healthcare ever works with patients and families to develop individualized care plans that support the patient'south wishes and values, and those plans include a discussion nearly the role of artificial nutrition and hydration.
How Family unit Members and Caregivers Tin can Assistance
A key gene that should guide decisions about diet and hydration at the end of life is patient choice. Patients who prefer quality of life at the end of life ofttimes desire to be unencumbered by tubes and equipment in their final hours, allowing them to be physically close to their family unit members and able to receive the comfort care they desire.
Family members and caregivers play an important function by supporting a loved one through the dying process:
- If the patient can still swallow or drink, offering pocket-sized sips of water/liquids, ice chips, hard candy or very small amounts of nutrient via spoon. Accept cues from the patient when to stop.
- If the patient can no longer drinkable, proceed the lips and oral cavity moist with swabs, a wet launder cloth, lip balm or moisturizers.
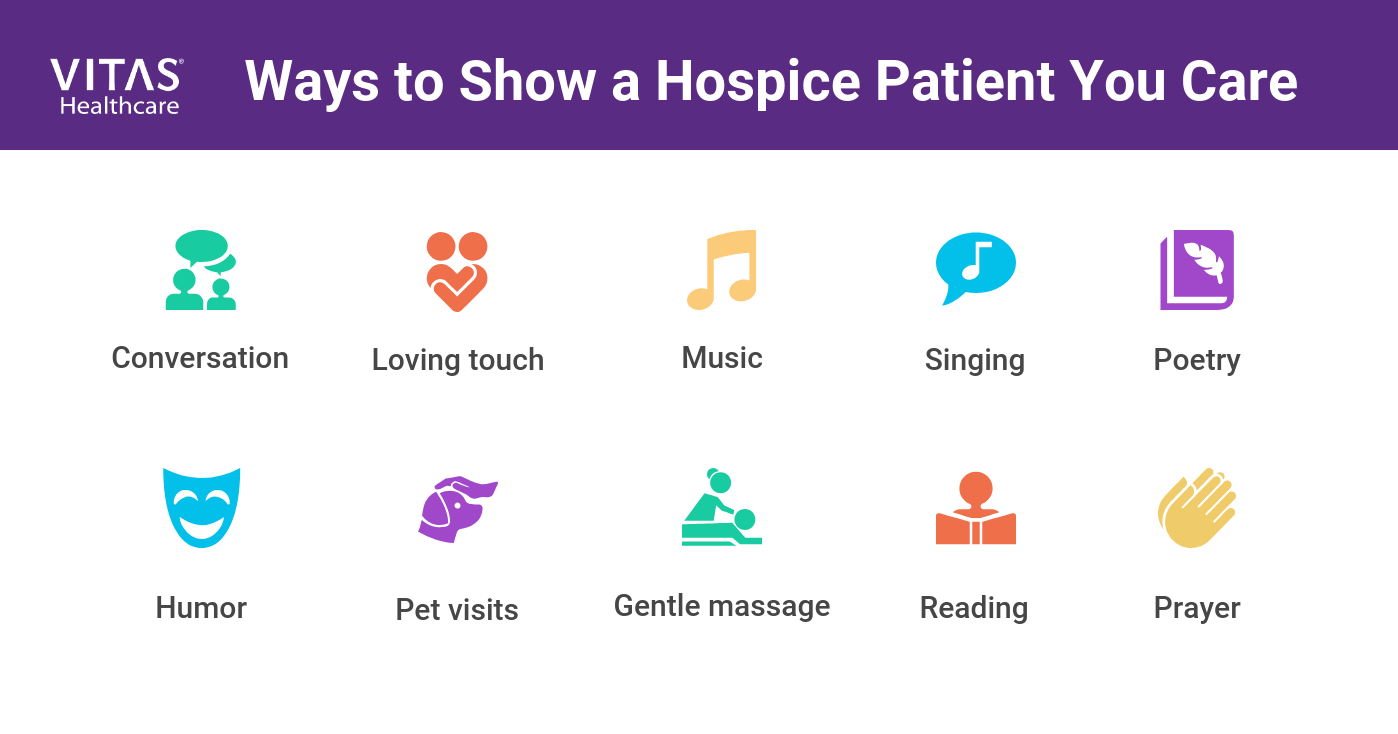
- If the patient can no longer eat or refuses to eat, provide culling forms of nourishment: conversation, loving touch, music, singing, poesy, humor, pet visits, gentle massage, reading, prayers or other acts of caring and honey.
Acknowledge Potential ANH Complications
Stop-of-life patients who are fed through artificial means tin suffer from gagging, tube complications (due east.g., blockages or infections), discomfort, aspiration pneumonia, pressure sores, bloating and a sense of "drowning" or feeling "trapped."
Moreover, studies have shown that artificial nutrition has very petty impact on survival for hospice patients. For example, studies evidence that dementia patients who are tube-fed take no different life expectancy than those who are slow hand-fed.
Craft and Honor a Compassionate End-of-Life Care Program
Ideally, decisions near care near the cease of life are made while anybody is good for you and able to speak their minds. That's when an advance directive should be written and shared with family and healthcare professionals.
The reality is that decisions are often put off until the patient is no longer able to communicate their wishes, leaving family members and a knowledgeable healthcare team to make decisions. Hospice professionals can offer specific types of care and support around diet and hydration for your loved 1 as death nears:
- The hospice squad will continue to relieve pain and manage symptoms
- The family's personal, cultural and religious beliefs and values around nutrition and hydration will be honored
- Family unit members and caregivers will be taught how to manage thirst and hunger compassionately and without artificial ways in a patient'southward final days of life
- In the final weeks, days and hours of life, families will exist reassured that the patient's decline and ultimate decease is due to the progression of the underlying disease procedure and not the natural decreasing and ultimate abeyance of eating and drinking.
The Challenge of Feeding Tubes
Hospice services will non be denied to a patient who already has a feeding tube in identify. The hospice team will work closely with the patient, family unit and caregiver to make up one's mind whether to go on to use the tube. While a feeding tube technically can exist removed, most often the conclusion is made to just end using information technology.
Feeding tubes typically are not placed in a patient who is terminally ill. But all necessary steps are taken to ensure comfort and pain relief every bit the end of life nears. In rare circumstances, the VITAS team might administer IV fluids temporarily to prevent dehydration or provide comfort, simply feeding and drinking will primarily exist done by mouth.
Source: https://www.vitas.com/family-and-caregiver-support/what-to-expect-from-hospice/when-a-hospice-patient-stops-eating-or-drinking
0 Response to "How Long Can an Elderly Person Live Without Eating"
Post a Comment